I recently had the privilege of attending the Dysautonomia International annual conference where healthcare practitioners, patients, and caregivers from all over the world came together for a weekend to connect and learn about the various facets of dysautonomia.
Dysautonomia, sometimes referred to as an invisible illness, is a highly under and/or misdiagnosed illness that affects millions of people world-wide. People suffering from dysautonomia often look perfectly healthy, and routine lab tests typically confirm this. However, on the inside their nervous system is raging war with their body.
Imagine if every time you stood up you had a bout of altitude sickness, or that minute odors, such as someone’s hand lotion, could set off an immune reaction. What if every day activities, such as vacuuming your house or walking your dog, took so much out of you that you were bedridden for days to weeks, living in a fog and unable to concentrate?
These are just a few of the challenges people suffering from dysautonomia might encounter.
Dysautonomia Defined: What you need to know
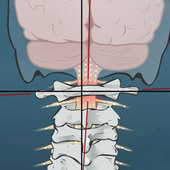
Dysautonomia refers to the dysfunction of your autonomic nervous system, the part of your nervous system that controls all the things that you don’t consciously think about. This includes processes like regulating your heart and breathing rate, secreting enzymes for digestion, controlling your body temperature, and influencing your sleep patterns. Some common symptoms of dysautonomia you might experience include:
- dizziness or lightheadedness
- brain fog
- headaches
- nausea
- digestive and/or reproductive troubles
- disturbed sleep
- temperature fluctuations
Though no one single cause has been identified, there is strong evidence that links the onset of autonomic dysfunction following an illness or infection, or a physical trauma, particularly concussions or whiplash type injuries.
Three Keys to Managing Your Dysautonomia
The weekend was jam-packed with valuable information and I want to share some of the top take-aways I gleaned from the incredible presenters and patients:
1. Dysautonomia does not affect one single system; it is a full body imbalance and a holistic approach to treatment must be taken.
2. Exercise is a critical piece to improving your body’s ability to adapt and respond to triggers that might create a flare-up in your symptoms.
For the average Joe this might sound like common sense, but for someone suffering from autonomic imbalance the thought of exercising can be a daunting challenge. If you are suffering from one of the various syndromes of dysautonomia, such as POTS (postural orthostatic tachycardia syndrome) or ME/CFS (myalgic encephalomyelitis/ chronic fatigue syndrome), you might find that recumbent exercises or aquatic exercises are easier to tolerate. This can include rowing exercises, recumbent bike exercises, or aqua therapy exercises. The key here is to set goals and be consistent. Change will not happen overnight, but think of this as an investment in the future you a year from now.
3. Early recognition and treatment can be a game changer.
The average time it takes for someone to be diagnosed with dysautonomia is approximately six years—this is WAY too long!
Taking a proactive approach when dealing with a sickness or head and neck injury can drastically reduce the risk of disability in the years to follow. Asking questions and being informed when it comes to your health can help facilitate speedier recognition and treatment.
Ask questions, be informed
Dysautonomia doesn’t need to be invisible. As more people learn about this often overlooked illness, better support and treatment systems can be created.
To learn more visit www.dysautonomiainternational.org or send us your questions.
Dr. Michelle Speranza
NUCCA Chiropractic
The Vital Posture™ Clinic
Calgary, Canada